Krok-2 Therapy Rheumatology Bases with Highlights & Explanations
The bellow material is aimed to improve the study and understanding of the Krok 2 Therapy Rheumatology with the use of highlights for relevant key works, links to rlevant study materials, reference images and explanations to individual questions aimed at making remembrance of questions easier and also understanding of new questions for the upcoming Step 2 exam.
Others complication of RA are;adverse effect of medications,felty syndrome,bakers cysts, Atlanto- axial sublaxation.
Note:–Heberden’s and Bouchard’s node are a sign of osteoarthritis and are caused by formation of osteophytes (calcific spurs) of the articular (joint) cartilage in response to repeated trauma at the joint.
EXP:-
EXP:-
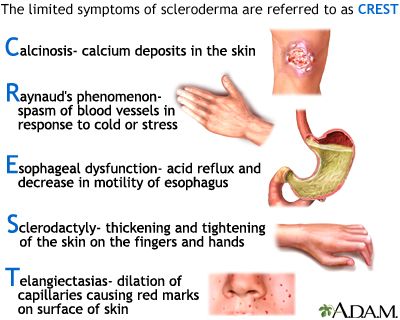
Note: face amimia, masked face, face like fish mouth associates with Systemic scleroderma,
EXP:-
EXP:-
- Your sex. Women are more likely than men to develop rheumatoid arthritis.
- Age. Rheumatoid arthritis can occur at any age, but it most commonly begins between the ages of 40 and 60.
- Family history. If a member of your family has rheumatoid arthritis, you may have an increased risk of the disease.
- Smoking. Cigarette smoking increases your risk of developing rheumatoid arthritis, particularly if you have a genetic predisposition for developing the disease. Smoking also appears to be associated with greater disease severity.
- Environmental exposures. Although uncertain and poorly understood, some exposures such as asbestos or silica may increase the risk for developing rheumatoid arthritis. Emergency workers exposed to dust from the collapse of the World Trade Center are at higher risk of autoimmune diseases such as rheumatoid arthritis.
- Obesity. People who are overweight or obese appear to be at somewhat higher risk of developing rheumatoid arthritis, especially in women diagnosed with the disease when they were 55 or younger.
- MORNING – Morning stiffness of >1 hour duration
- Always – Arthritis of atleast three areas ( PIP, MCP, MTP, WRIST etc.)
- Helps – Hand arthritis
- See* – Symmetrical arthritis
- Nature – Nodules as observed by physician
- Fresh – rheumatoid Factor &
- RADIANT – Radiological changes
EXP:-
Patient diagnosed as rheumaroid arthritis so best diagnosis for RA is roentgenography of hands.Rheumatoid arthritis(RA) a chronic progressive disease causing inflammation in the joints and resulting in painful deformity and immobility, especially in the fingers, wrists, feet, and ankles.Female affected more than male. MCPs and PIPs involved but not DIPs. Characterized by morning stiffness more than 1hr, pain gradually reliefs after exercis , ulnar deviation, Boutonierre deformity ,Swan neck deformity ,rheumatoid nodules backers cysts also present.
- Your sex. Women are more likely than men to develop rheumatoid arthritis.
- Age. Rheumatoid arthritis can occur at any age, but it most commonly begins between the ages of 40 and 60.
- Family history. If a member of your family has rheumatoid arthritis, you may have an increased risk of the disease.
- Smoking. Cigarette smoking increases your risk of developing rheumatoid arthritis, particularly if you have a genetic predisposition for developing the disease. Smoking also appears to be associated with greater disease severity.
- Environmental exposures. Although uncertain and poorly understood, some exposures such as asbestos or silica may increase the risk for developing rheumatoid arthritis. Emergency workers exposed to dust from the collapse of the World Trade Center are at higher risk of autoimmune diseases such as rheumatoid arthritis.
- Obesity. People who are overweight or obese appear to be at somewhat higher risk of developing rheumatoid arthritis, especially in women diagnosed with the disease when they were 55 or younger.
- MORNING – Morning stiffness of >1 hour duration
- Always – Arthritis of atleast three areas ( PIP, MCP, MTP, WRIST etc.)
- Helps – Hand arthritis
- See* – Symmetrical arthritis
- Nature – Nodules as observed by physician
- Fresh – rheumatoid Factor &
- RADIANT – Radiological changes
31.) A 32-year-old male patient has beensuffering from pain in the sacrum and coxofemoral joints,
- Your sex. Women are more likely than men to develop rheumatoid arthritis.
- Age. Rheumatoid arthritis can occur at any age, but it most commonly begins between the ages of 40 and 60.
- Family history. If a member of your family has rheumatoid arthritis, you may have an increased risk of the disease.
- Smoking. Cigarette smoking increases your risk of developing rheumatoid arthritis, particularly if you have a genetic predisposition for developing the disease. Smoking also appears to be associated with greater disease severity.
- Environmental exposures. Although uncertain and poorly understood, some exposures such as asbestos or silica may increase the risk for developing rheumatoid arthritis. Emergency workers exposed to dust from the collapse of the World Trade Center are at higher risk of autoimmune diseases such as rheumatoid arthritis.
- Obesity. People who are overweight or obese appear to be at somewhat higher risk of developing rheumatoid arthritis, especially in women diagnosed with the disease when they were 55 or younger.
- MORNING – Morning stiffness of >1 hour duration
- Always – Arthritis of atleast three areas ( PIP, MCP, MTP, WRIST etc.)
- Helps – Hand arthritis
- See* – Symmetrical arthritis
- Nature – Nodules as observed by physician
- Fresh – rheumatoid Factor &
- RADIANT – Radiological changes
- Your sex. Women are more likely than men to develop rheumatoid arthritis.
- Age. Rheumatoid arthritis can occur at any age, but it most commonly begins between the ages of 40 and 60.
- Family history. If a member of your family has rheumatoid arthritis, you may have an increased risk of the disease.
- Smoking. Cigarette smoking increases your risk of developing rheumatoid arthritis, particularly if you have a genetic predisposition for developing the disease. Smoking also appears to be associated with greater disease severity.
- Environmental exposures. Although uncertain and poorly understood, some exposures such as asbestos or silica may increase the risk for developing rheumatoid arthritis. Emergency workers exposed to dust from the collapse of the World Trade Center are at higher risk of autoimmune diseases such as rheumatoid arthritis.
- Obesity. People who are overweight or obese appear to be at somewhat higher risk of developing rheumatoid arthritis, especially in women diagnosed with the disease when they were 55 or younger.
- MORNING – Morning stiffness of >1 hour duration
- Always – Arthritis of atleast three areas ( PIP, MCP, MTP, WRIST etc.)
- Helps – Hand arthritis
- See* – Symmetrical arthritis
- Nature – Nodules as observed by physician
- Fresh – rheumatoid Factor &
- RADIANT – Radiological changes
- Your sex. Women are more likely than men to develop rheumatoid arthritis.
- Age. Rheumatoid arthritis can occur at any age, but it most commonly begins between the ages of 40 and 60.
- Family history. If a member of your family has rheumatoid arthritis, you may have an increased risk of the disease.
- Smoking. Cigarette smoking increases your risk of developing rheumatoid arthritis, particularly if you have a genetic predisposition for developing the disease. Smoking also appears to be associated with greater disease severity.
- Environmental exposures. Although uncertain and poorly understood, some exposures such as asbestos or silica may increase the risk for developing rheumatoid arthritis. Emergency workers exposed to dust from the collapse of the World Trade Center are at higher risk of autoimmune diseases such as rheumatoid arthritis.
- Obesity. People who are overweight or obese appear to be at somewhat higher risk of developing rheumatoid arthritis, especially in women diagnosed with the disease when they were 55 or younger.
- MORNING – Morning stiffness of >1 hour duration
- Always – Arthritis of atleast three areas ( PIP, MCP, MTP, WRIST etc.)
- Helps – Hand arthritis
- See* – Symmetrical arthritis
- Nature – Nodules as observed by physician
- Fresh – rheumatoid Factor &
- RADIANT – Radiological changes
Note: Libman–Sacks endocarditis associated with SLE
- Your sex. Women are more likely than men to develop rheumatoid arthritis.
- Age. Rheumatoid arthritis can occur at any age, but it most commonly begins between the ages of 40 and 60.
- Family history. If a member of your family has rheumatoid arthritis, you may have an increased risk of the disease.
- Smoking. Cigarette smoking increases your risk of developing rheumatoid arthritis, particularly if you have a genetic predisposition for developing the disease. Smoking also appears to be associated with greater disease severity.
- Environmental exposures. Although uncertain and poorly understood, some exposures such as asbestos or silica may increase the risk for developing rheumatoid arthritis. Emergency workers exposed to dust from the collapse of the World Trade Center are at higher risk of autoimmune diseases such as rheumatoid arthritis.
- Obesity. People who are overweight or obese appear to be at somewhat higher risk of developing rheumatoid arthritis, especially in women diagnosed with the disease when they were 55 or younger.
- MORNING – Morning stiffness of >1 hour duration
- Always – Arthritis of atleast three areas ( PIP, MCP, MTP, WRIST etc.)
- Helps – Hand arthritis
- See* – Symmetrical arthritis
- Nature – Nodules as observed by physician
- Fresh – rheumatoid Factor &
- RADIANT – Radiological changes
- Your sex. Women are more likely than men to develop rheumatoid arthritis.
- Age. Rheumatoid arthritis can occur at any age, but it most commonly begins between the ages of 40 and 60.
- Family history. If a member of your family has rheumatoid arthritis, you may have an increased risk of the disease.
- Smoking. Cigarette smoking increases your risk of developing rheumatoid arthritis, particularly if you have a genetic predisposition for developing the disease. Smoking also appears to be associated with greater disease severity.
- Environmental exposures. Although uncertain and poorly understood, some exposures such as asbestos or silica may increase the risk for developing rheumatoid arthritis. Emergency workers exposed to dust from the collapse of the World Trade Center are at higher risk of autoimmune diseases such as rheumatoid arthritis.
- Obesity. People who are overweight or obese appear to be at somewhat higher risk of developing rheumatoid arthritis, especially in women diagnosed with the disease when they were 55 or younger.
- MORNING – Morning stiffness of >1 hour duration
- Always – Arthritis of atleast three areas ( PIP, MCP, MTP, WRIST etc.)
- Helps – Hand arthritis
- See* – Symmetrical arthritis
- Nature – Nodules as observed by physician
- Fresh – rheumatoid Factor &
- RADIANT – Radiological changes
- Your sex. Women are more likely than men to develop rheumatoid arthritis.
- Age. Rheumatoid arthritis can occur at any age, but it most commonly begins between the ages of 40 and 60.
- Family history. If a member of your family has rheumatoid arthritis, you may have an increased risk of the disease.
- Smoking. Cigarette smoking increases your risk of developing rheumatoid arthritis, particularly if you have a genetic predisposition for developing the disease. Smoking also appears to be associated with greater disease severity.
- Environmental exposures. Although uncertain and poorly understood, some exposures such as asbestos or silica may increase the risk for developing rheumatoid arthritis. Emergency workers exposed to dust from the collapse of the World Trade Center are at higher risk of autoimmune diseases such as rheumatoid arthritis.
- Obesity. People who are overweight or obese appear to be at somewhat higher risk of developing rheumatoid arthritis, especially in women diagnosed with the disease when they were 55 or younger.
- MORNING – Morning stiffness of >1 hour duration
- Always – Arthritis of atleast three areas ( PIP, MCP, MTP, WRIST etc.)
- Helps – Hand arthritis
- See* – Symmetrical arthritis
- Nature – Nodules as observed by physician
- Fresh – rheumatoid Factor &
- RADIANT – Radiological changes
- Your sex. Women are more likely than men to develop rheumatoid arthritis.
- Age. Rheumatoid arthritis can occur at any age, but it most commonly begins between the ages of 40 and 60.
- Family history. If a member of your family has rheumatoid arthritis, you may have an increased risk of the disease.
- Smoking. Cigarette smoking increases your risk of developing rheumatoid arthritis, particularly if you have a genetic predisposition for developing the disease. Smoking also appears to be associated with greater disease severity.
- Environmental exposures. Although uncertain and poorly understood, some exposures such as asbestos or silica may increase the risk for developing rheumatoid arthritis. Emergency workers exposed to dust from the collapse of the World Trade Center are at higher risk of autoimmune diseases such as rheumatoid arthritis.
- Obesity. People who are overweight or obese appear to be at somewhat higher risk of developing rheumatoid arthritis, especially in women diagnosed with the disease when they were 55 or younger.
- MORNING – Morning stiffness of >1 hour duration
- Always – Arthritis of atleast three areas ( PIP, MCP, MTP, WRIST etc.)
- Helps – Hand arthritis
- See* – Symmetrical arthritis
- Nature – Nodules as observed by physician
- Fresh – rheumatoid Factor &
- RADIANT – Radiological changes
- Your sex. Women are more likely than men to develop rheumatoid arthritis.
- Age. Rheumatoid arthritis can occur at any age, but it most commonly begins between the ages of 40 and 60.
- Family history. If a member of your family has rheumatoid arthritis, you may have an increased risk of the disease.
- Smoking. Cigarette smoking increases your risk of developing rheumatoid arthritis, particularly if you have a genetic predisposition for developing the disease. Smoking also appears to be associated with greater disease severity.
- Environmental exposures. Although uncertain and poorly understood, some exposures such as asbestos or silica may increase the risk for developing rheumatoid arthritis. Emergency workers exposed to dust from the collapse of the World Trade Center are at higher risk of autoimmune diseases such as rheumatoid arthritis.
- Obesity. People who are overweight or obese appear to be at somewhat higher risk of developing rheumatoid arthritis, especially in women diagnosed with the disease when they were 55 or younger.
- MORNING – Morning stiffness of >1 hour duration
- Always – Arthritis of atleast three areas ( PIP, MCP, MTP, WRIST etc.)
- Helps – Hand arthritis
- See* – Symmetrical arthritis
- Nature – Nodules as observed by physician
- Fresh – rheumatoid Factor &
- RADIANT – Radiological changes